Breast Cancer Screening & What Scan is Right For You
Andrea Ahlm has been walking through the doors of RAYUS Radiology for the past 20 years for her annual mammogram – without fail.
“It’s just one of those things that I know is in my best interest to do. I have friends who have had breast cancer and early detection has been the thing that has prevented them from having greater problems.”
“It’s simple, it’s painless and it’s a good thing to have done,” says Andrea.
Since 1989, breast cancer mortality rates have been decreasing, with women under 50 experiencing the largest decrease. According to Breastcancer.org, this decrease is thought to be the direct result of the advancements made in treatment, as well as early detection through screening and increased awareness.
Over the past several years, breast cancer screening modalities and options for preventative surgeries have been big news. Angelina Jolie wrote an article for the New York Times about her decision to have a double mastectomy after learning, through a blood test, that she carries the BRCA1 gene, which increases the risk of developing breast cancer as well as ovarian cancer. Her decision, as she states in a follow-up article, was very personal and a direct reflection of her family history of breast and ovarian cancer. It was also the result of preventative screenings she went through. Much like Andrea Ahlm, Angelina knew that preventative screening measures could save her life. And most importantly, she knew her decision would be based on what was right for her as an individual.
What is right for you?
When you come to RAYUS Radiology for a breast exam, we start with a lot of questions and a look at your own personal and family health history. Dr. Hayley Sheldon, a breast and body radiologist explains:
“We do a comprehensive risk assessment analysis based on a two or three-page questionnaire that the patients fill out. We then run a risk assessment if a few risk factors are triggered, such as a sister or mother with breast cancer or late age for childbirth or no children.”
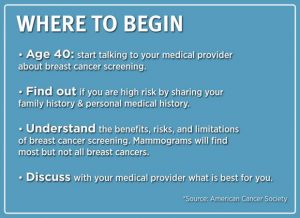
Depending on risk factors identified at your first appointment, a personal protocol is put in place. It’s personal, Dr. Sheldon says, because there is no one test that’s best for every patient and every situation. This is why it is important for you to schedule your screening mammogram, talk with your medical team, and understand what is available to you.
Breast Cancer Screening: The First Exam
The first step to preventing breast cancer is to schedule your appointment for a mammogram. Mammograms are the most common imaging test and have been proven in many studies to be an effective way to detect cancer early in all patients. This is why mammograms are commonly used for screening purposes starting at age 40. If you do not have symptoms and are not identified as high risk, you will be following a simple screening protocol, which includes a yearly mammogram.
Mammograms use very small, safe doses of radiation. But if you are concerned, there are low-dose mammography units available. Make sure to check with your radiology center to see what your options are when you schedule your appointment.
Breast Cancer Screening: More Options
If you have a family history of breast cancer, dense breast tissue (which is identified by your radiologist at your initial appointment), or other risk factors, there are supplementary imaging options for your screening protocol. These options include breast ultrasound, automated breast ultrasound and 3-D digital tomography, which are all non-invasive and help to diagnose abnormalities and detect breast cancer early.
Your radiologist will make recommendations as to what type of supplemental screening is right for you based on your initial screening mammogram, personal and family history, risk factors, and tissue density.
Some women also get breast MRI exams. In 2007, the American Cancer Society and American College of Radiology came out with recommendations that the MRI’s higher sensitivity is a good screening tool for women who are at a higher risk. You’re considered “high risk” if you have a 20-25% or greater overall lifetime risk of developing breast cancer. Carrie Riccobono, a clinical nurse specialist at Froedtert RAYUS Radiology Breast Care in Milwaukee, says for certain women, regular breast MRI is recommended:
“A breast MRI is a great diagnostic tool for the right woman and when I say the right woman, what do I mean? If you’ve got really dense breasts, if you have a history of breast cancer and they want to do surveillance to see if the breast is changing, you can do it in addition to a mammogram.”
An MRI is not an ideal screening test for everyone, but for high-risk patients, annual mammograms and MRIs are recommended to get the fullest picture.
Using Imaging to Diagnose Breast Cancer
All of these options – a mammogram, an ultrasound, 3-D digital tomography and MRI – are like tools in a tool kit. They can be used in combination to solve the problem of a diagnostic procedure and target any mass for biopsy. So why wouldn’t you get it done?
According to the National Breast Cancer Foundation, 60-70% of women with breast cancer have no connection to known risk factors. This is why it is vitally important for you to schedule a yearly mammogram starting at age 40. Talk to your doctor about what screening is right for you and come back every year, just like Andrea Ahlm. When asked about her annual mammogram routine, Andrea said, “It’s simple, it’s painless, and it’s a good thing to have done.” We couldn’t have said it better ourselves.